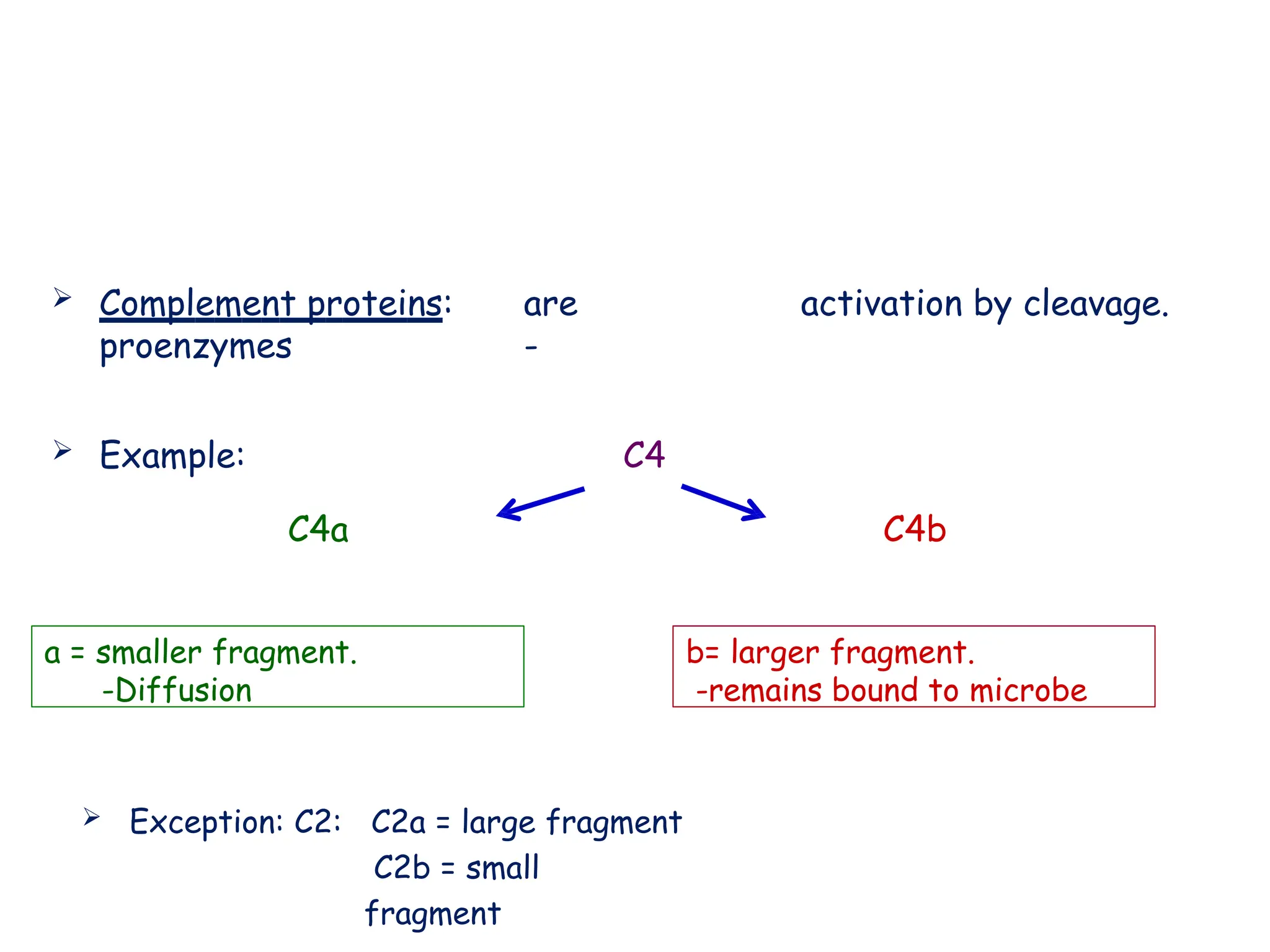
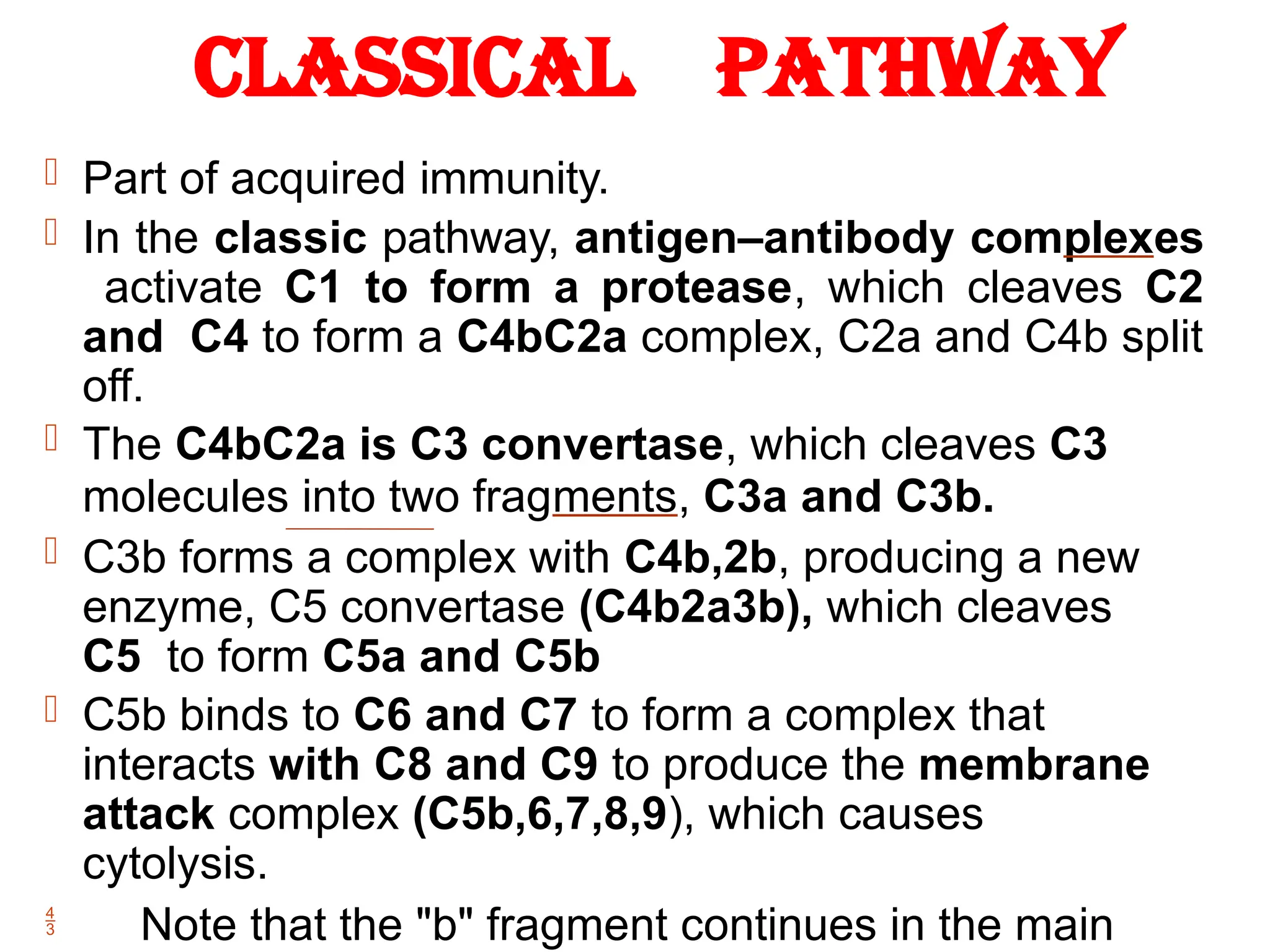
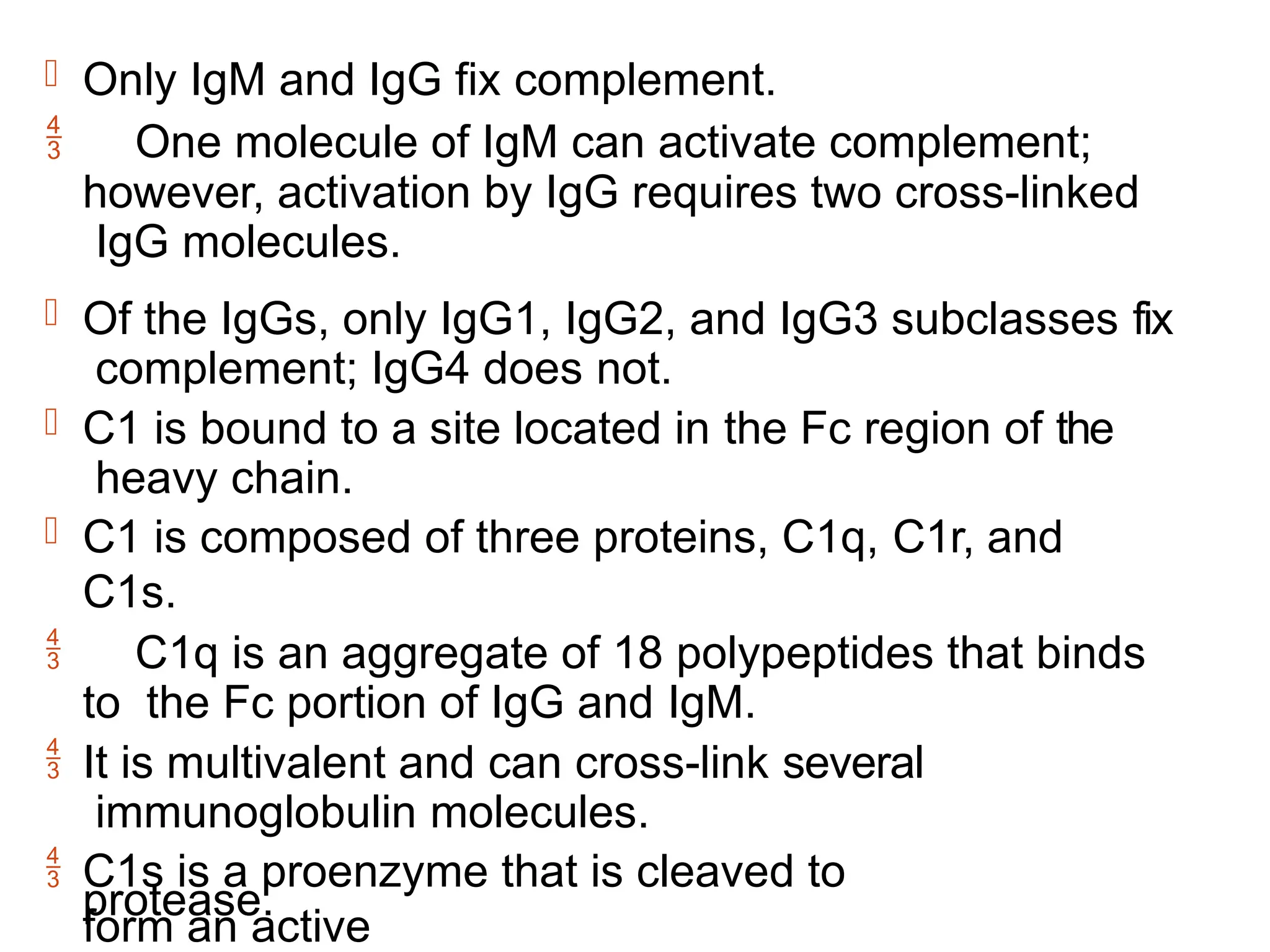
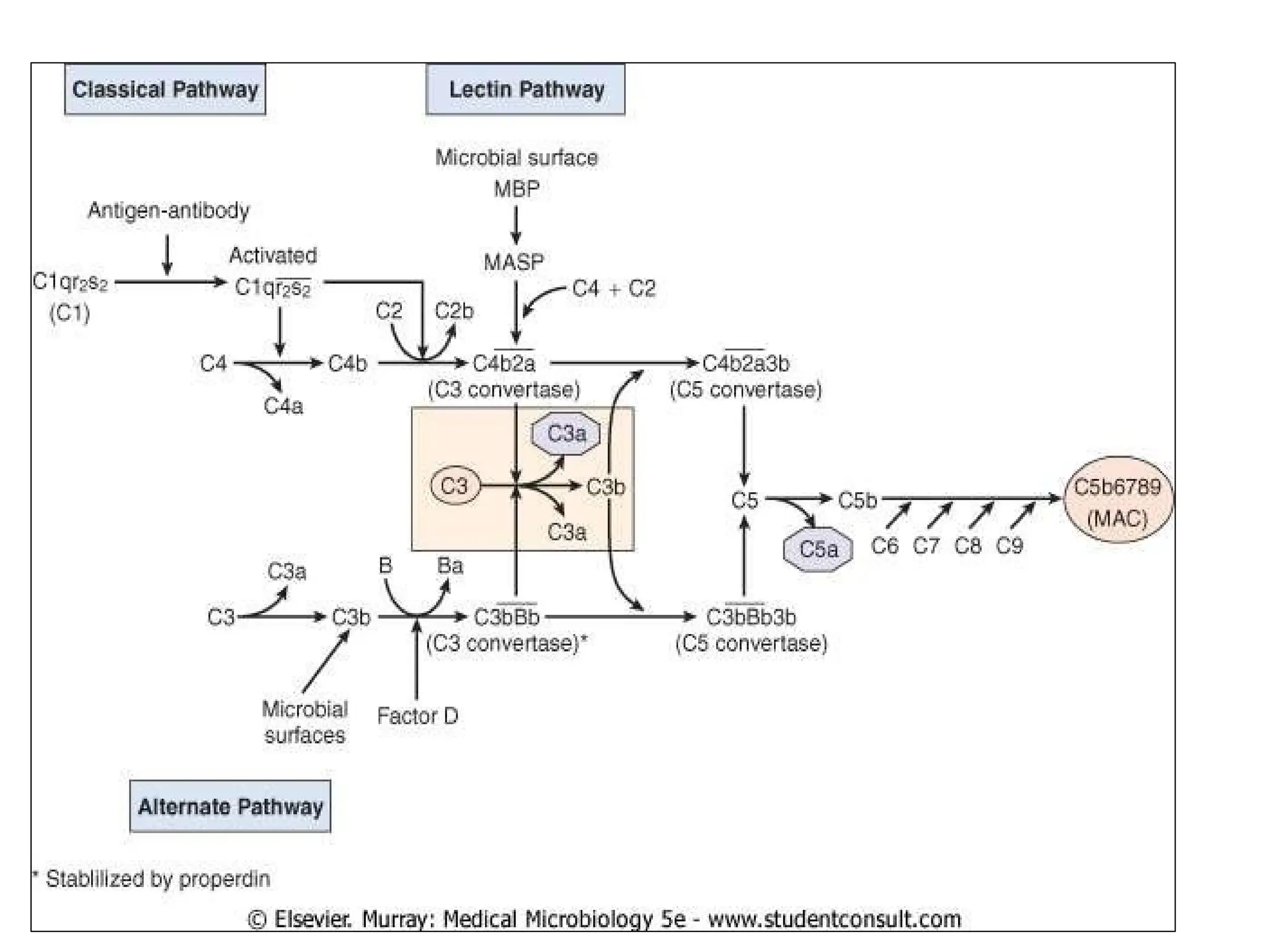
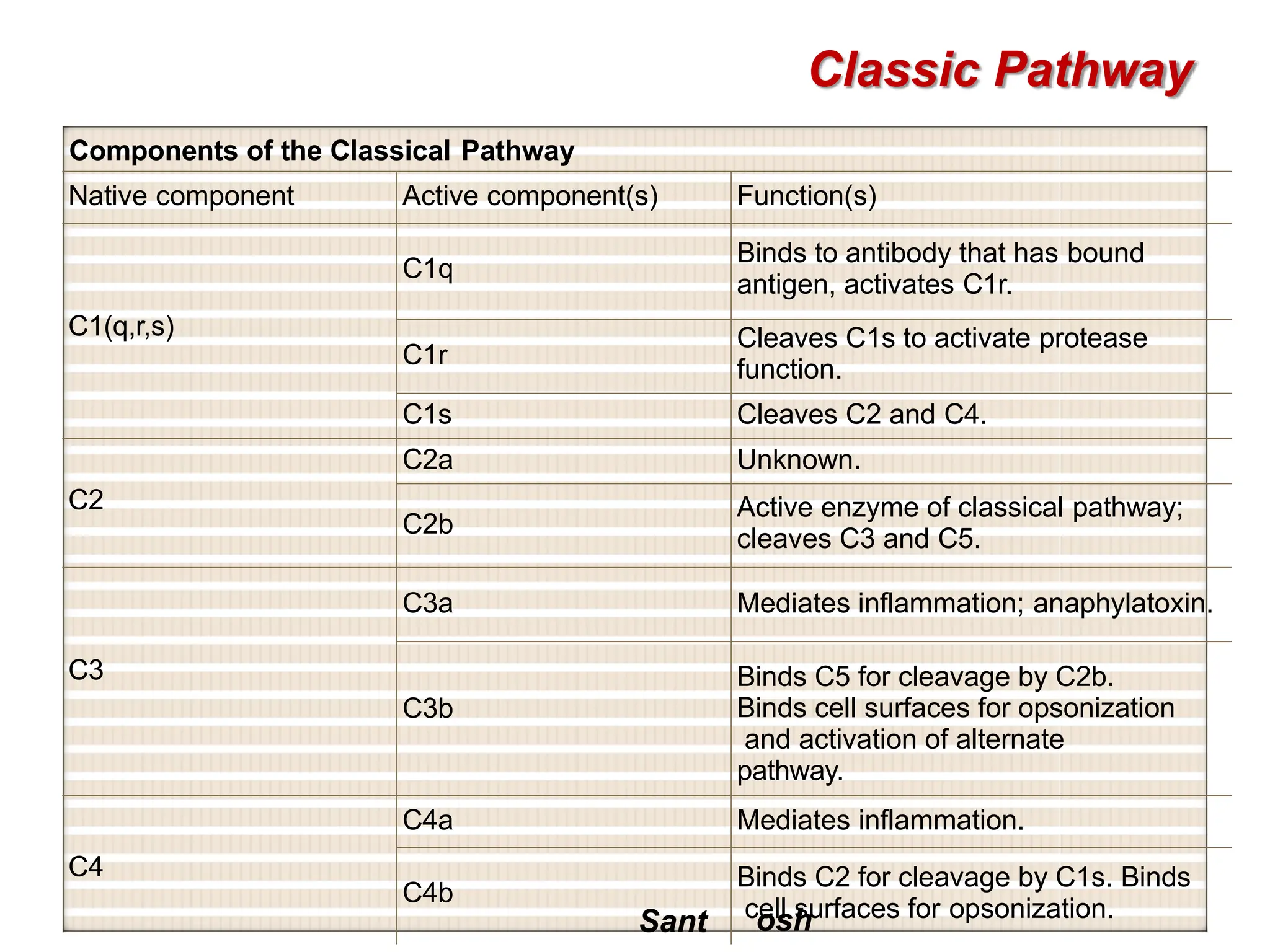
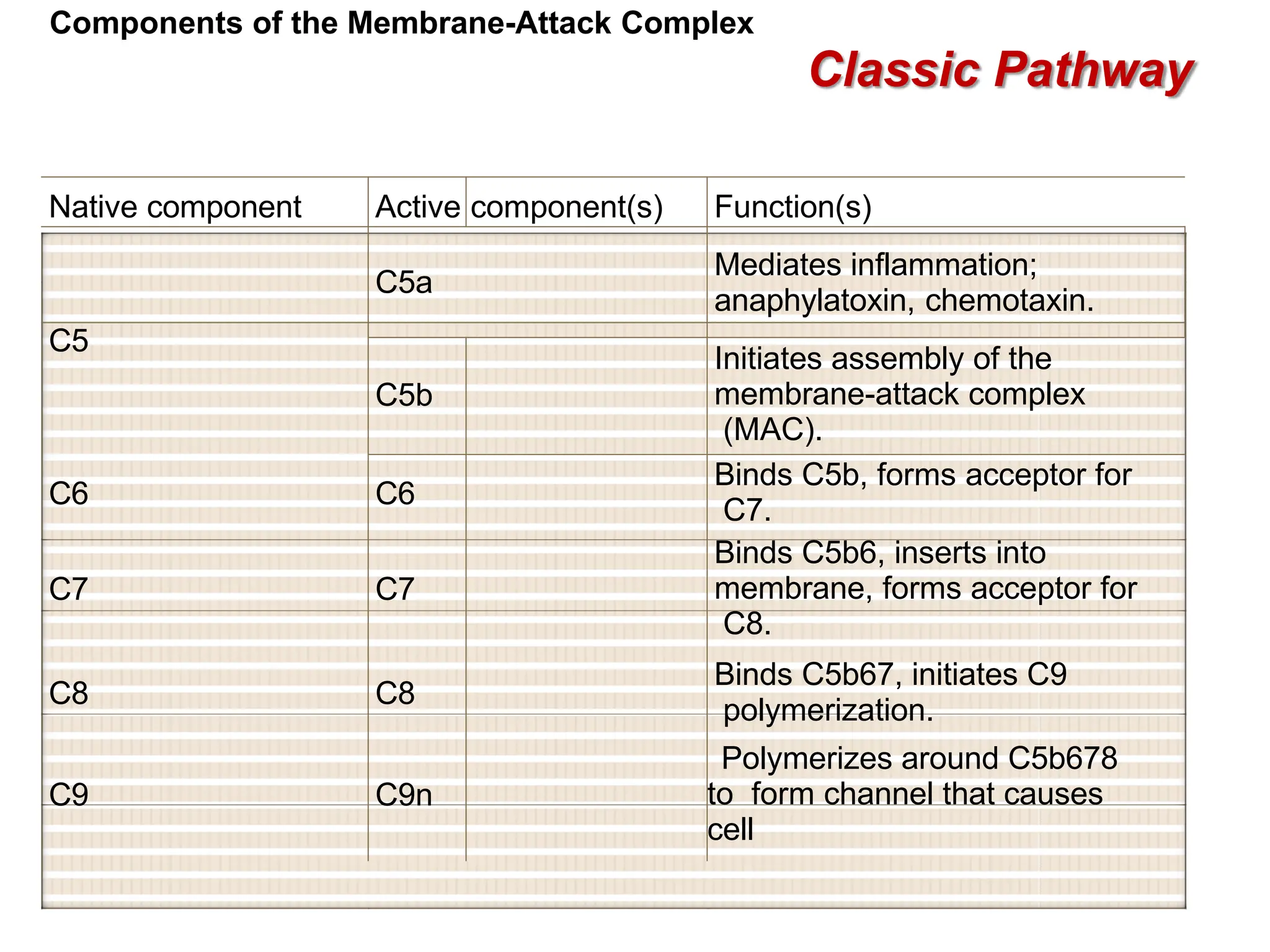
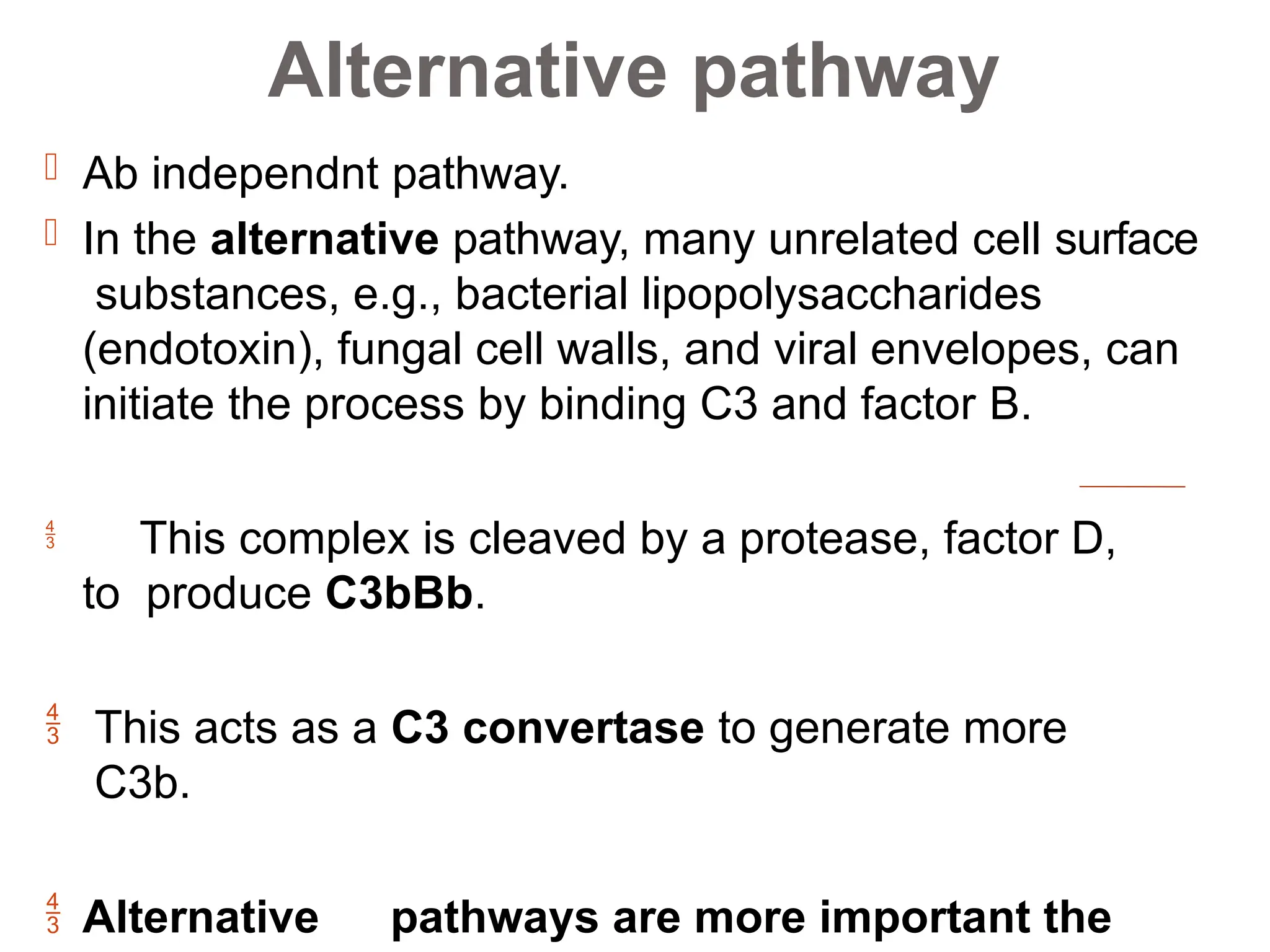
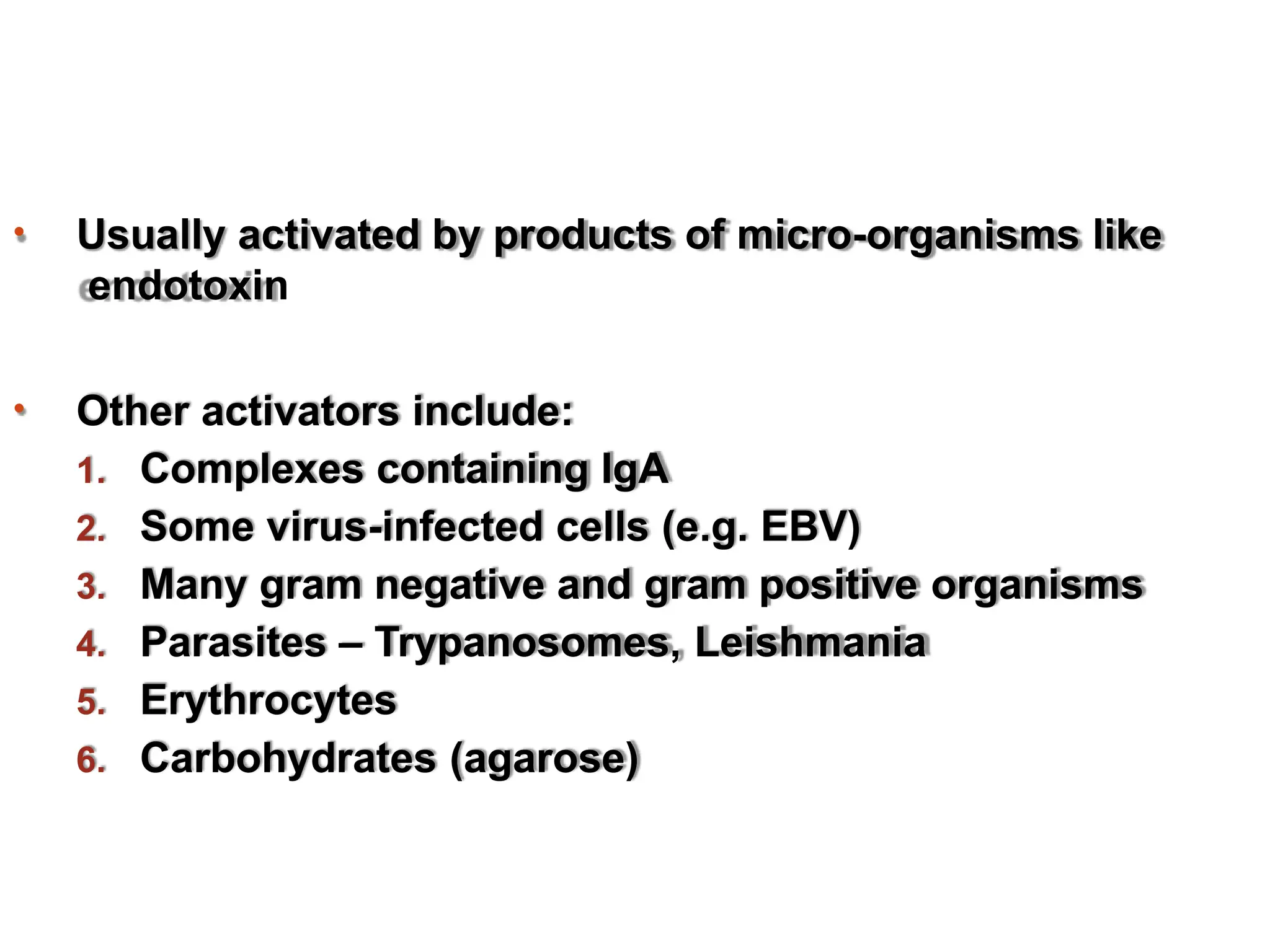
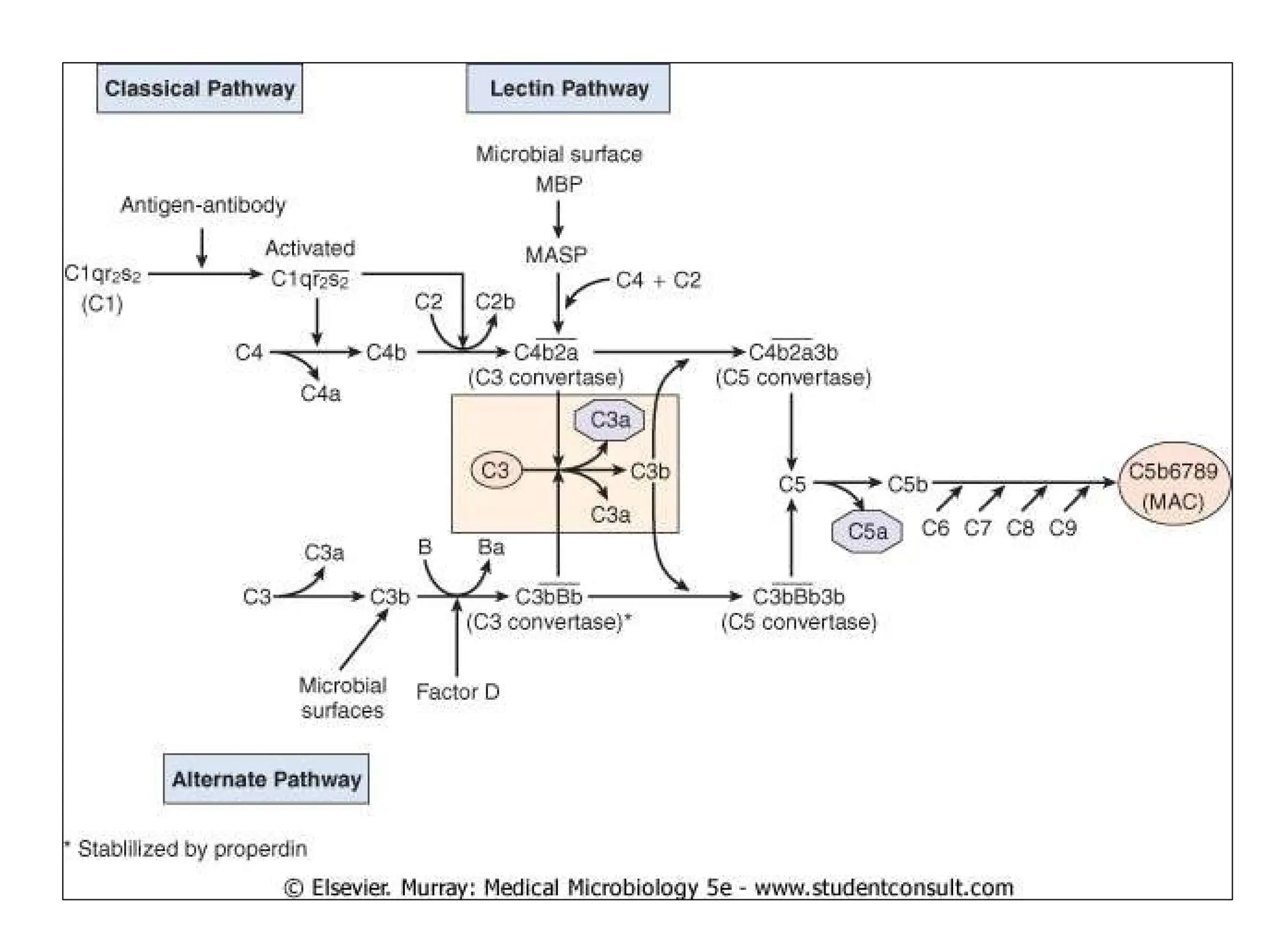
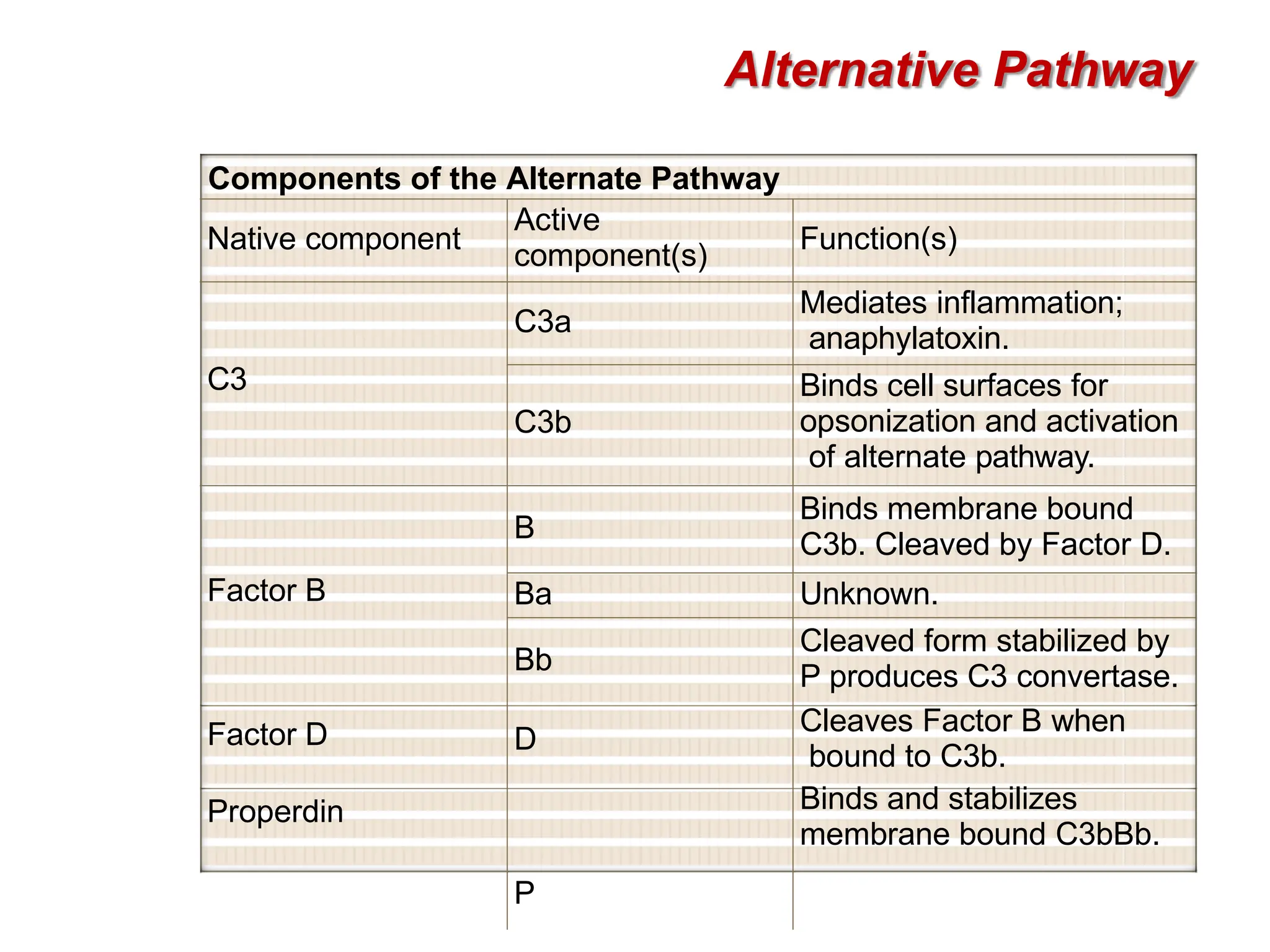
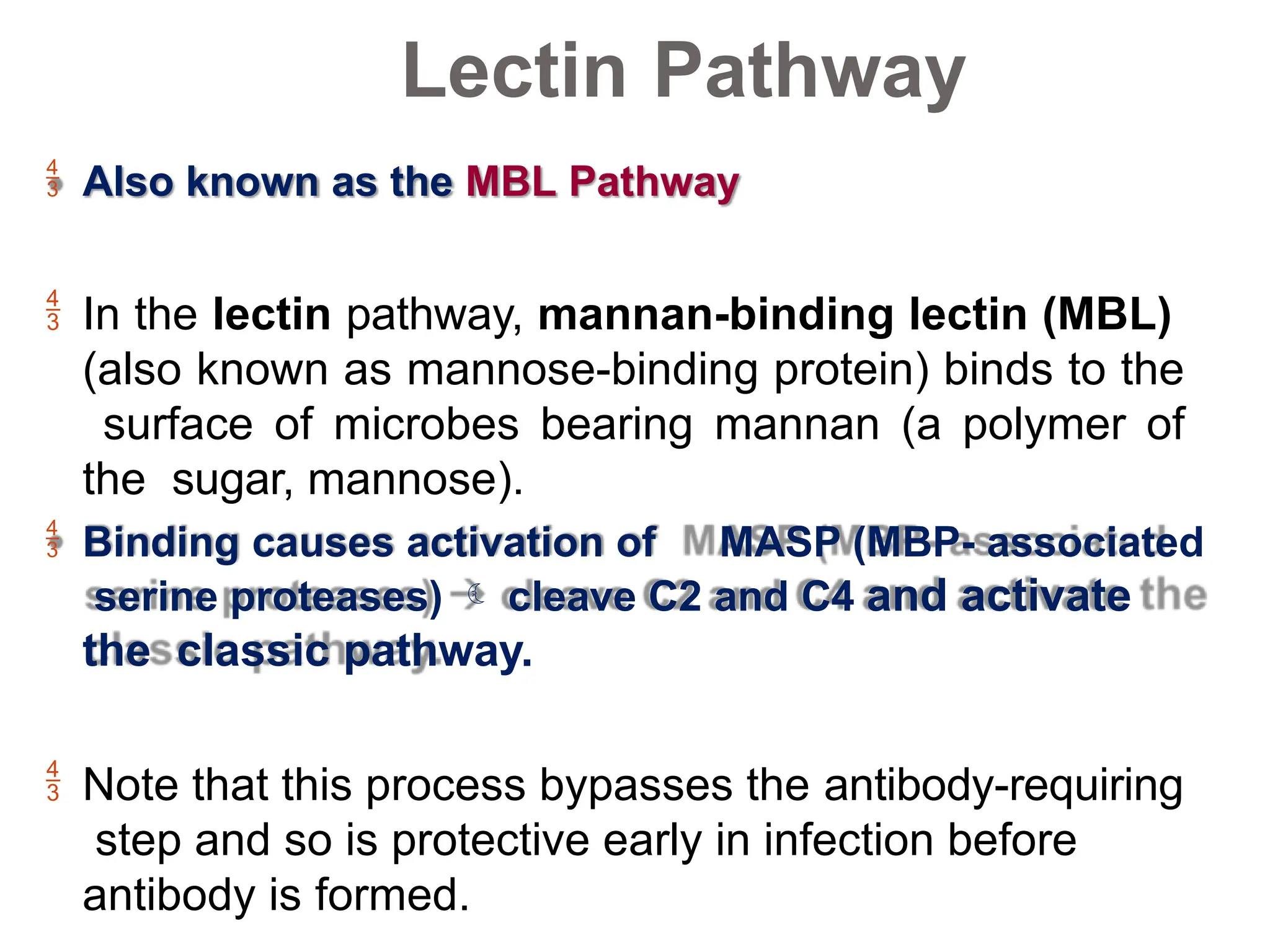
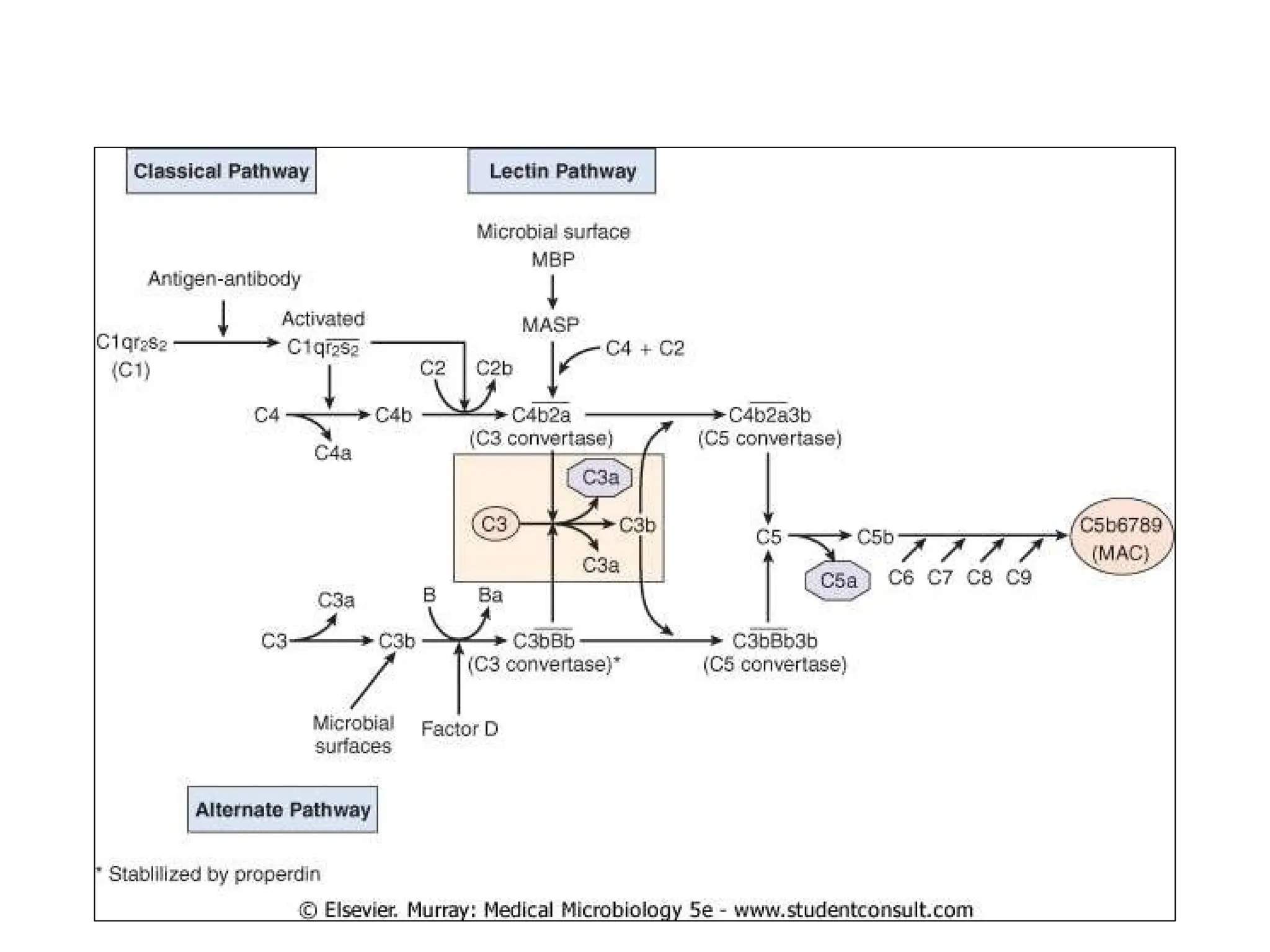
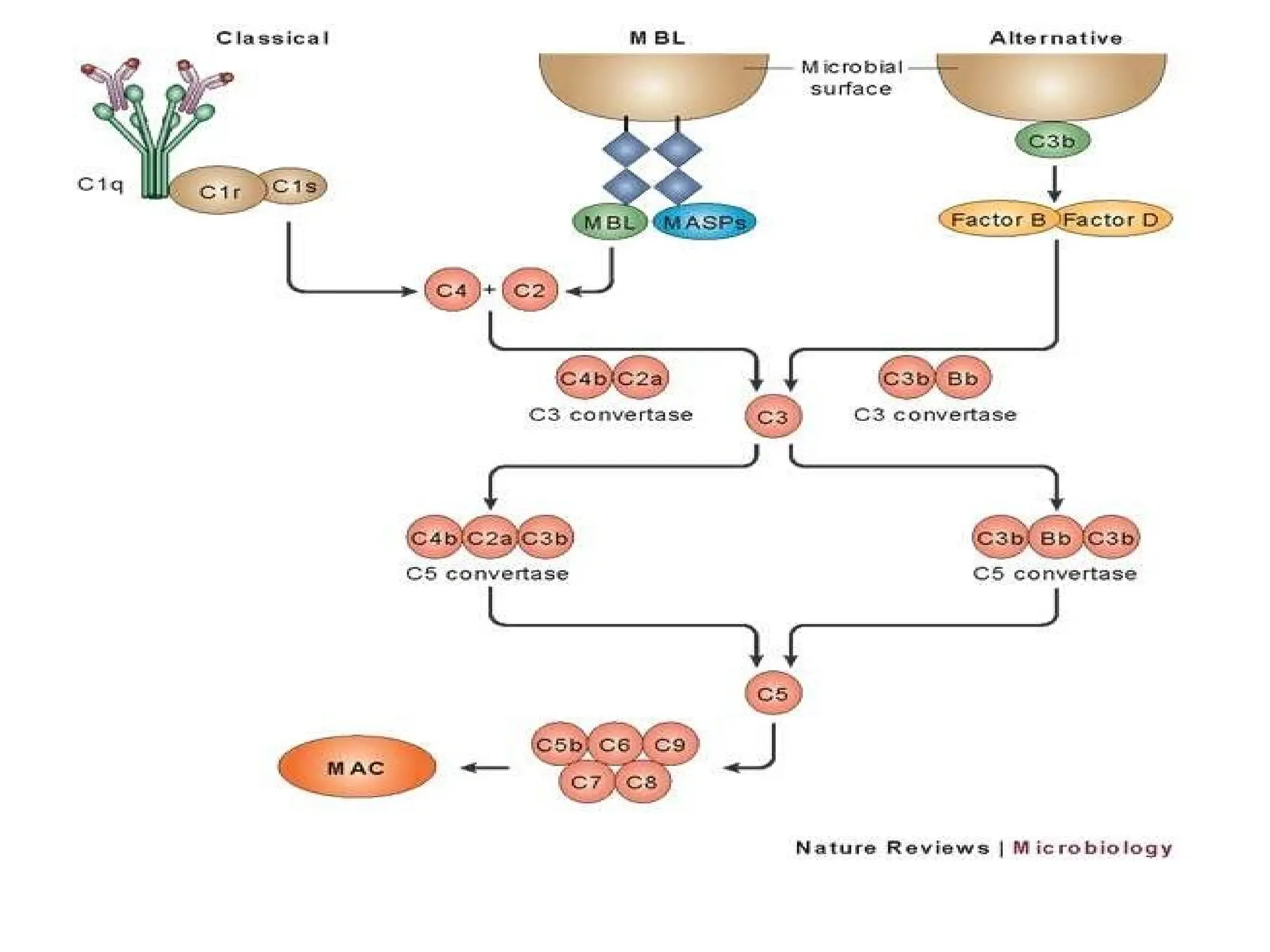
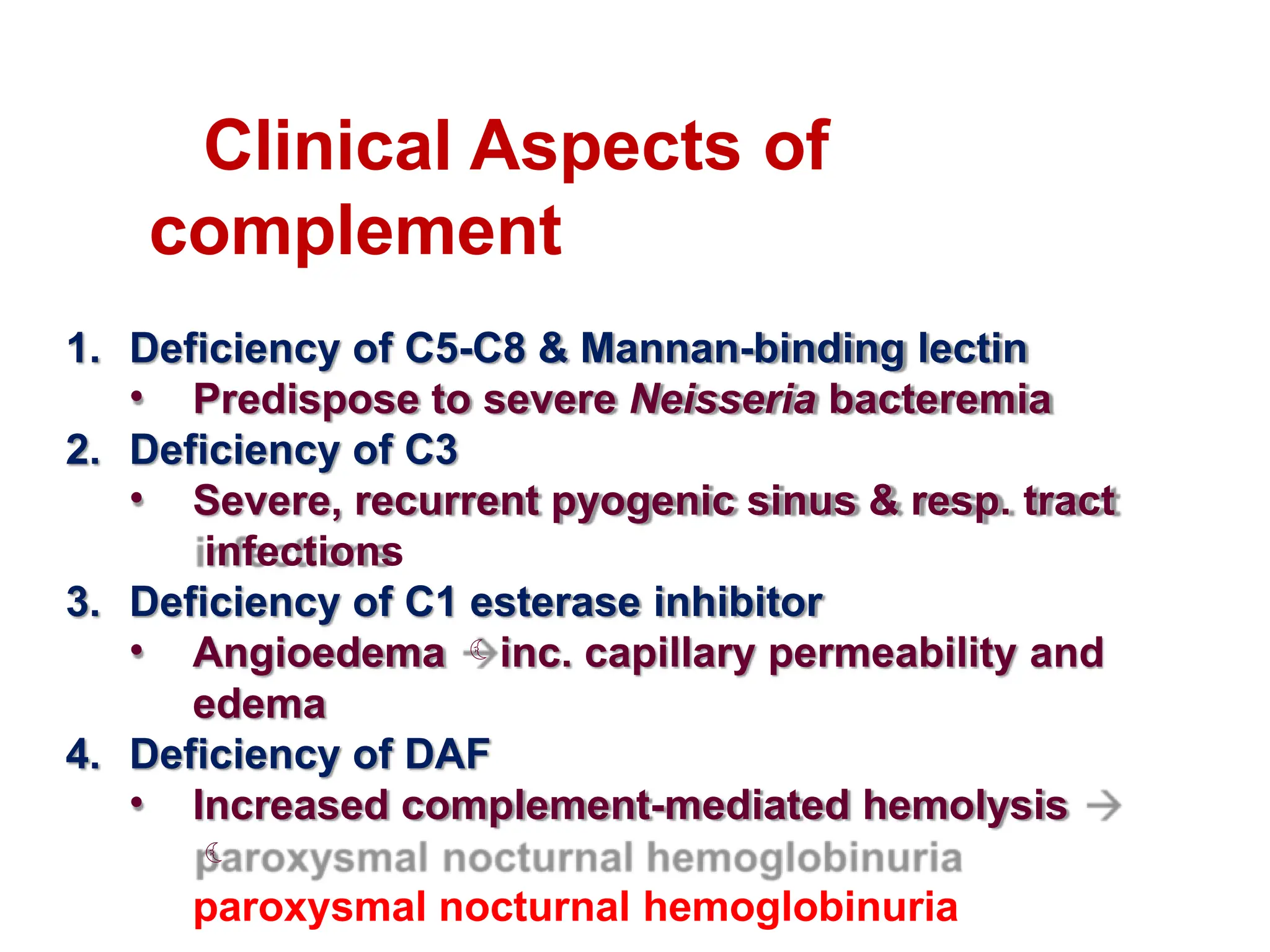
The complement system is a group of approximately 30 proteins that enhance the immune response and play crucial roles in both innate and adaptive immunity, primarily functioning through three activation pathways: classical, alternative, and lectin. Activated via proteolysis, these proteins facilitate the lysis of pathogens, generate inflammation mediators, and promote opsonization. Deficiencies or dysregulation within this system can lead to increased susceptibility to infections and various autoimmune disorders.