Percutaneous stabilization can increase mobility without disrupting cancer treatment
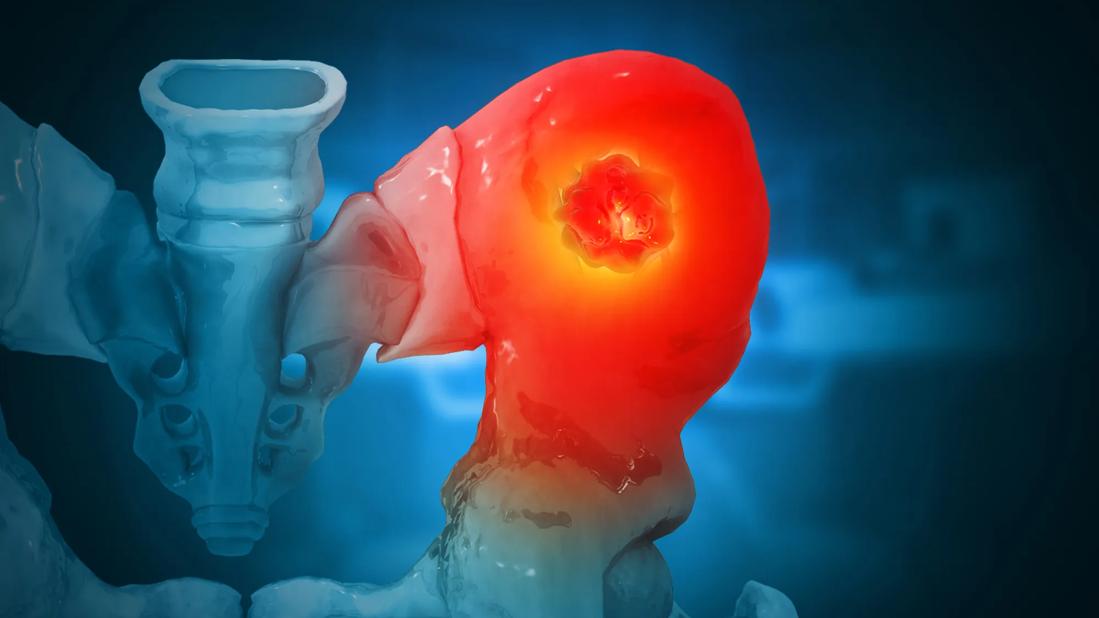
Patients with metastatic disease of the acetabulum now have a minimally invasive option for surgically stabilizing the bone to reduce pain, improve mobility and prevent further fracture. Percutaneous stabilization is becoming more prevalent thanks to advances in imaging techniques, surgical instrumentation and implants, says Lukas Nystrom, MD, a Cleveland Clinic orthopaedic surgeon who specializes in musculoskeletal oncology.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“This minimally invasive approach can both treat and fill metastatic lesions, reinforcing the bone and making it less likely to break, while causing little to no disruption in chemotherapy or other cancer treatments,” he says.
Formerly, when cancer spread to the acetabulum, treatment options were restricted to:
For these reasons, the orthopaedic oncology community has a growing interest in percutaneous stabilization techniques for the acetabulum.
“We’re finding that we can positively impact patients’ lives with this innovative approach that works well in conjunction with cancer treatments,” Dr. Nystrom says. “These techniques are less invasive and don’t present the same concerns as a larger open surgery.”
The procedure is performed in an operating room, with the patient under general anesthesia. The surgeon uses imaging guidance to identify trajectories for implanting screws or performing kyphoplasty to fill space and stabilize bone. Using a tripod concept, the surgeon stabilizes the hip socket through three incisions, each approximately 1 cm.
Advertisement

This fixation procedure can be combined with cryoablation of the lesion by an interventional radiology team. However, often the lesion is not removed but rather treated with radiation or other therapies directed by the oncology team.
Despite the less invasive nature, the procedure is not without risk.
“Percutaneous stabilization is a technically demanding procedure in a high-risk surgical territory,” Dr. Nystrom says. “It requires careful assessment of imaging and surgical precision to avoid misdirecting a screw into the bowel, bladder or blood vessels, for example.”
Percutaneous stabilization should be considered for any patient who has a large metastatic lesion in the acetabulum that is causing pain or presenting a risk of fracture.
“It may not be appropriate for addressing smaller lesions or lesions that are more responsive to oncologic treatments, such as multiple myeloma, lymphoma and treatment-naïve breast cancer,” Dr. Nystrom says. “While the procedure is minimally invasive, it does carry some surgical risk. That risk may be avoided if a bone pathology can be eliminated through other, nonsurgical therapies.”
The procedure is not advised for patients unable to have general anesthesia or who have a very limited prognosis related to their overall disease. On the other hand, some patients have lesions that are so extensive or destructive that a larger open surgery is still required. Cleveland Clinic’s orthopaedic oncology team personalizes treatment recommendations based on each patient’s therapeutic goals and prognosis.
Advertisement
“Percutaneous stabilization is an option for many patients at risk of pathologic acetabular fracture,” Dr. Nystrom adds, “especially if they are experiencing pain. We’re available to help evaluate those patients and determine if surgical treatment is appropriate.”
Advertisement
Advertisement

Study shows that postop function is closer to normal than with total hip arthroplasty

New guidelines update recommendations

High-risk procedure prepares patient for lifesaving heart surgery

Simple score uses clinical factors to identify patients who might benefit from earlier screening

Cleveland Clinic is among the first in the U.S. to perform the procedure

Use of GLP-1s and improving cardiovascular health lowers risk of hematologic malignancies

Largest study of its kind identifies three treatment exposures that contribute to risk

Insights to help orthopaedic practices comply with the 2025 CMS mandate